Asthma is a chronic disease that makes your lungs very sensitive and can make it hard to breathe. Asthma can’t be cured, but with proper treatment, people with asthma can lead normal, active lives.
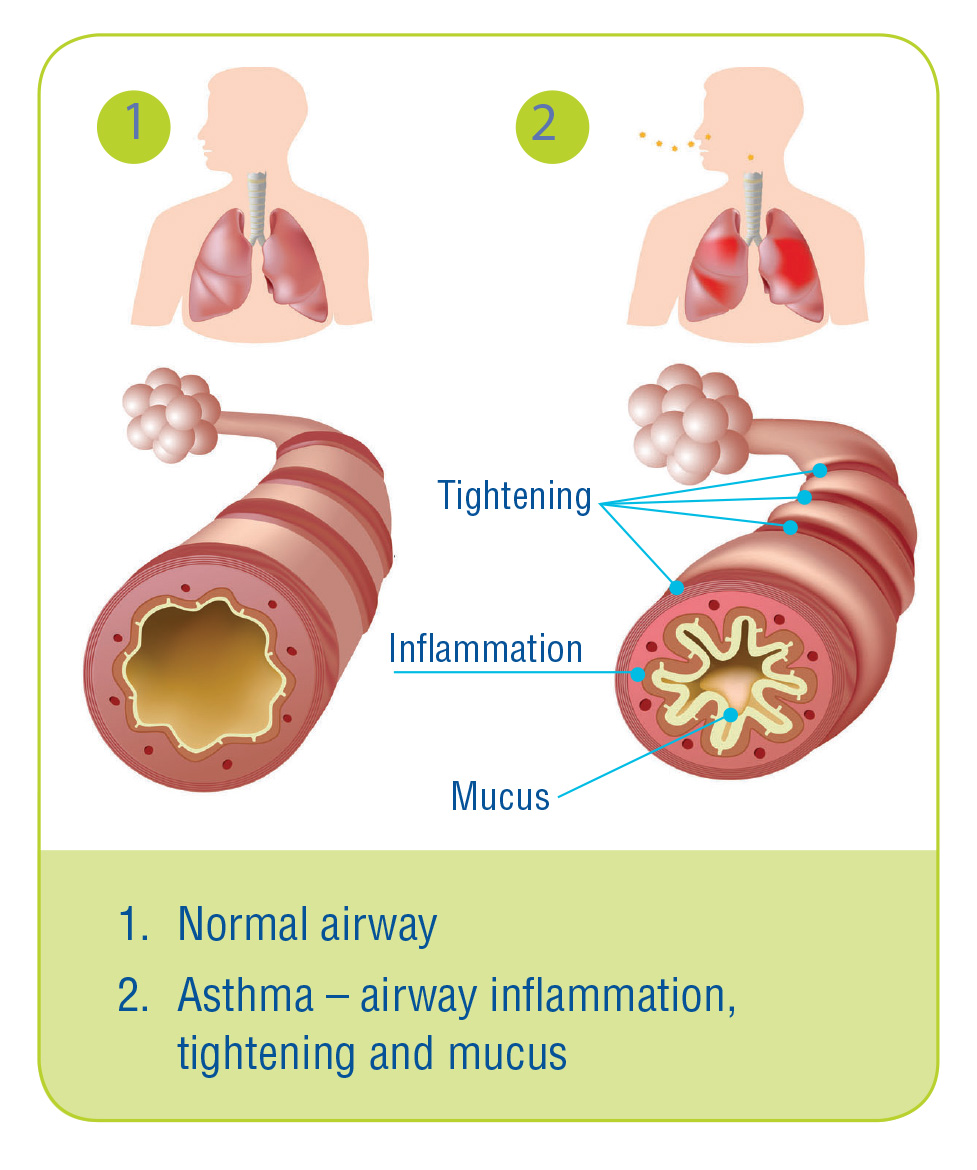
Certain things can make your airways become swollen and filled with mucus. The swelling and mucus makes your airways narrower, so it is hard for air to pass through.
Asthma may also cause your airways to become small and tight. This makes your airways narrower and makes it hard for air to pass through.